Dowager’s hump is described as excessive kyphotic curvature in the thoracic spine with a Cobb angle of more than 40 degrees. This case report presents a 61 years old female office clerk who experienced headaches and neck pain for 3 years that extended into her right shoulder and upper chest. She consulted her primary care physician two months before seeing the chiropractor when the neck pain worsened. A diagnosis of cervicalgia related to osteoarthritis was made based on cervical and thoracic X-ray findings. The patient received non-steroid anti-inflammatory drugs (celecoxib and etoricoxib) and stretching exercises at home. At the onset of chiropractic care, radiographs showed loss of cervical lordosis, narrowing at the C4-5, C5-C6, and C6-7 intervertebral disc space with marginal osteophytes. Based on these findings, a working diagnosis of cervicogenic headache was established. After treatment for 9 months, the patient showed improvement in symptoms and function from cervical curve radiographic change and dextro-convexity of the thoracic spine. Avoiding forward head flexion and maintaining correct posture in daily activities will be key mechanisms to prevent the reoccurrence of Dowager’s hump. The improvement of symptoms following chiropractic therapy has been shown to correlate with radiographic markers of spinal realignment.
Osteoporotic vertebral fractures are frequently misdiagnosed or under-recognized in the older population, leading to disease progression and reduced quality of life. This case of an 87-year-old woman with acute back pain highlights the importance of early diagnosis and management of fragility fractures. During the coronavirus disease (COVID-19) pandemic, patients with a history of well-managed osteoporosis experienced worsening symptoms of vertebral collapse due to activity limitations and prolonged immobilization. The initial diagnosis of spinal stenosis delayed appropriate treatment for four months. Serial magnetic resonance imaging revealed compression fractures at L1 and L3, and a dual-energy x-ray absorptiometry scan showed osteoporosis with a T-score of −3.2. Pharmacological therapy, including bisphosphonates, was initiated. A comprehensive rehabilitation program with a multidisciplinary approach, with bracing, and lifestyle changes helped stabilize the spine, reduce pain, and maximized function. Her condition improved with close monitoring and guidance during home exercises. This case exemplifies the necessity of a precise and timely diagnosis of osteoporotic vertebral fractures to initiate management and mitigate disease progression.
Text neck syndrome is a growing concern in the pediatric population due to the increased use of mobile devices and screens, potentially leading to long-lasting musculoskeletal issues. This case report presents a six-year-old boy with a one-month history of cephalgia and cervicalgia, who initially received insufficient care. After nine months of chiropractic intervention, the patient reported significant improvements in pain relief, neck mobility, and neurological symptoms, supported by radiographic findings. This report emphasizes the importance of early recognition and intervention in pediatric patients, as well as the role of ergonomics, exercise, and proper smartphone usage habits in preventing text neck and maintaining spinal health.
Keywords: direct primary care, chiropractic management, chiropractic, chiropractic therapy, primary care medicine, prevention in primary care, primary medical care
Cervicogenic angina and dyspnea are conditions characterized by chest discomfort and breathing difficulties that resemble angina pectoris and dyspnea of cardiac origin. However, this condition is caused by cervical spine pathology, cervical spondylosis, and radiculopathy. This case study reports a 66-year-old man who presented with cervicogenic angina and dyspnea due to cervical radiculopathy to a chiropractic clinic. The patient underwent a comprehensive diagnostic evaluation, including taking the patient’s history, a physical examination, and radiological investigations, which demonstrated cervical spine involvement consistent with a cervicogenic origin of the pain. The patient’s angina-like symptoms and dyspnea improved significantly after chiropractic manipulation of the spine, soft tissue mobilization, and other manual therapies. Accurate diagnosis is essential to minimize unnecessary cardiac interventions and ensure proper therapy for underlying cervical spine problems. This case demonstrates the necessity of conservative management, such as chiropractic care, for patients presenting with cervicogenic angina and dyspnea, particularly when a diagnostic assessment reveals cervical spinal involvement.

Abstract
Patient: Male, 45-year-old
Final Diagnosis: Cervical facet syndrome • radiation induced fibrosis
Symptoms: Headache • neck pain and stiffness
Medication: —
Clinical Procedure: Neck stretches • soft tissue manipulation • spinal manipulation • therapeutic ultrasound
Specialty: Chiropractic • Rehabilitation
Objective:
Rare disease
Background:
Pineal gland tumors are rare central nervous system tumors, and while neck pain and headaches may be common among those who have had these tumors removed, there is little research regarding management of these symptoms.
Case Report:
A 45-year-old man with a history of pineal germinoma treated with pinealectomy, chemotherapy, radiation therapy, and ventriculoperitoneal shunt placement at age 21 presented with chronic neck pain and headaches, which initially improved following his surgery and concurrent therapies, yet progressively worsened over the following years. He required thyroid and testosterone medication because of radiation-induced hypopituitarism, yet was employed, and until recently, active with playing tennis. He had previously seen his primary care provider, orthopedist, and neurologist, and had been cleared of severe pathology via brain magnetic resonance imaging and was referred to the chiropractor. On examination, the patient had severely limited passive cervical spine range of motion, yet hat no neurologic deficits, and radiographs showed mild cervical spondylosis and cervicothoracic scoliosis. His history and presentation were suggestive of radiation-induced fibrosis. The patient’s neck pain, headaches, and quality of life improved with multimodal treatments including spinal and soft-tissue manipulation, stretches, and yoga.
Conclusions:
This case illustrates long-term sequelae of a pineal gland tumor and its treatment, including neck pain and headache, and improvement with multimodal chiropractic therapies. Despite the success in this case, these results are not broadly generalizable. Further research is needed to understand the natural history of symptoms and effectiveness of multimodal therapies among patients who have had pineal tumor surgery.
Keywords: Chiropractic, Manipulation, Spinal, Neck Pain, Pineal Gland, Radiotherapy
Patient: Male, 45-year-old
Final Diagnosis: Cervical facet syndrome • radiation induced fibrosis
Symptoms: Headache • neck pain and stiffness
Medication: —
Clinical Procedure: Neck stretches • soft tissue manipulation • spinal manipulation • therapeutic ultrasound
Specialty: Chiropractic • Rehabilitation
Objective:
Rare disease
Background:
Pineal gland tumors are rare central nervous system tumors, and while neck pain and headaches may be common among those who have had these tumors removed, there is little research regarding management of these symptoms.
Case Report:
A 45-year-old man with a history of pineal germinoma treated with pinealectomy, chemotherapy, radiation therapy, and ventriculoperitoneal shunt placement at age 21 presented with chronic neck pain and headaches, which initially improved following his surgery and concurrent therapies, yet progressively worsened over the following years. He required thyroid and testosterone medication because of radiation-induced hypopituitarism, yet was employed, and until recently, active with playing tennis. He had previously seen his primary care provider, orthopedist, and neurologist, and had been cleared of severe pathology via brain magnetic resonance imaging and was referred to the chiropractor. On examination, the patient had severely limited passive cervical spine range of motion, yet hat no neurologic deficits, and radiographs showed mild cervical spondylosis and cervicothoracic scoliosis. His history and presentation were suggestive of radiation-induced fibrosis. The patient’s neck pain, headaches, and quality of life improved with multimodal treatments including spinal and soft-tissue manipulation, stretches, and yoga.
Conclusions:
This case illustrates long-term sequelae of a pineal gland tumor and its treatment, including neck pain and headache, and improvement with multimodal chiropractic therapies. Despite the success in this case, these results are not broadly generalizable. Further research is needed to understand the natural history of symptoms and effectiveness of multimodal therapies among patients who have had pineal tumor surgery.
Keywords: Chiropractic, Manipulation, Spinal, Neck Pain, Pineal Gland, Radiotherapy
简介:
Adjacent segment pathology (ASP) refers to degenerative changes at segments immediately contiguous to previous spinal fusion. Its pathophysiology is hypothesized as being possibly due to altered biomechanical stresses on adjacent levels following spinal fusion or due to patient propensity to develop progressive degenerative change. This case report describes a 61-year-old female who presented with neck pain and cervical radiculopathy attributed to an anterior cervical discectomy and spinal fusion performed for degenerative disc disease 30 years earlier. ASP was seen on magnetic resonance imaging (MRI) and radiograph. Treatment consisted of cervical manipulation, soft-tissue mobilization, flexion-distraction decompression, and therapeutic ultrasound to release restriction and restore muscle strength. Following 34 sessions of chiropractic intervention, her symptoms were resolved. Patients with ASP will have ongoing shared care between general practitioners and secondary or tertiary care pain units. This report aims to build a shared understanding from the wider vision of ASP and help primary practitioners to manage ASP effectively.
Key words: Adjacent segment pathology; chiropractic manipulation; degenerative change; spinal fusion
Introduction: Adjacent segment pathology (ASP) refers to degenerative changes observed at functional spinal units adjacent to the site of previous fusion procedure.[1] All spinal surgeries altering motion across a joint can contribute to additional stress and mechanical loads on the segments immediately above and below the surgery site and accelerate subsequent degeneration. These conditions can compress nerves in the spine, causing pain and additional conditions like radiculopathy and myelopathy. ASP can be complicated by age-related changes, anatomical disruption, surgical technique, malalignment of the spine, and preexisting comorbidities (e.g., degenerative spondylosis, osteoporosis, diabetes mellitus, and smoking).[23]
The accelerated degeneration of the adjacent segments could be a multisegmental problem and can be challenging to manage. This article will enhance readers understanding of ASP and help primary practitioners to manage ASP effectively. This case report has been prepared after obtaining written informed consent from the patient to have the case details and accompanying images published. Owing to the nature of the retrospective chart review, IRB approval is not required.
Case Report: A 61-year-old female presented with severe neck pain that radiated into the right shoulder and upper arm for 2 months duration. The patient described experiencing the same symptoms 30 years earlier and was treated successfully with C5-C6 and C6-C7 anterior cervical discectomy and fusion. Following surgical intervention, the patient experienced approximately 20 years of symptomatic improvement, but the patient observed progressive deterioration of her condition over the past 10 years and had been followed by her orthopedic surgeon. Two months prior to presentation, the patient experienced rapid deterioration of her neck pain, which was associated with numbness, radiating pain, and weakness of the right arm. She had attempted 20 sessions of physical therapy with minimal relief.
Discussion:
ASP is recognized by clinicians as a debilitating condition characterized by axial pain and radiculopathy after spinal fusion. The progression of ASP can result from compressive loading on the adjacent segments and the compromised nutrient diffusion in the intervertebral discs after segment fusion.[4] Biomechanical and clinical data have demonstrated that motion preservation technologies minimize stresses placed on adjacent functional segments.[2] The latest data suggested that positive effects after artificial disc replacement are found in terms of a reduced incidence of ASP and reoperation as compared with anterior cervical discectomy and interbody fusion procedures.[25]
The radiographic changes of the adjacent segments include osteophyte formation, disc degeneration, foraminal narrowing, spinal stenosis, spinal instability, and scoliosis.[6] As in all degenerative conditions, the goals of ASP treatment are to alleviate pain, strengthen paravertebral musculature, improve range of motion, limit progressive changes, and avoid unnecessary surgery. Apart from physical suffering, persistent pain has clear emotional and behavioral consequences that have an impact on the outcome of treatment. With proper instruction and support, psychological approaches can improve pain management outcomes.
General practitioners have a key role to play in securing better outcomes for their patients. Patients can have both nociceptive and neuropathic pain and will have ongoing shared care between general practitioners and secondary or tertiary care pain units. It is inappropriate to place total reliance on further surgery. Multidisciplinary care allows patients to receive coordinated support and comprehensive care. Nonsurgical treatments such as medications, physiotherapy, manipulative therapy, psychotherapy, and nerve stimulation/modulation techniques can be helpful in most spine symptoms. Minimally invasive surgery is reserved for ASP patients with gradual emergence of neurological deficits.[7] However, there are no comparative studies on the efficacy of conservative treatment versus surgical treatment.[8] The current study aims to share an understanding of tasks between primary and secondary care for alleviating musculoskeletal pains like ASP.
Conclusion: Presented is a case of symptomatic ASP after anterior cervical discectomy and spinal fusion. Appropriate conditioning and proper retrieval of biomechanical elasticity can allow the spine to function properly. Conservative treatments should always be contemplated as an alternative method for ASP patients before resorting to surgery.
1. Donnally CJ 3rd, Patel PD, Canseco JA, Divi SN, Goz V, Sherman MB, et al Current incidence of adjacent segment pathology following lumbar fusion versus motion-preserving procedures:A systematic review and meta-analysis of recent projections Spine J 2020 20 1554–65
5. Findlay C, Ayis S, Demetriades AK Total disc replacement versus anterior cervical discectomy and fusion:A systematic review with meta-analysis of data from a total of 3160 patients across 14 randomized controlled trials with both short- and medium- to long-term outcomes Bone Joint J 2018 100-B 991–1001
7. Kapetanakis S, Gkantsinikoudis N, Gkasdaris G, Charitoudis G Treatment of adjacent segment disease with percutaneous transforaminal endoscopic discectomy:Early experience and results J Orthop Surg (Hong Kong) 2020 28 2309499020960560
Clinical features: The painful symptoms were associated with a great impact on the sleep and routine tasks during the month preceding the first presentation to the practitioner. The patient scored an 84% on the Neck Disability Index (NDI). Spinal palpation revealed restricted range of motion at C2/3, C4/5, C5/6, T1/2, T3/4 and T7/8 vertebral segments. Radiographic evaluation of the cervical spine revealed reduced cervical lordosis with Cobb angle 3°.
Intervention and outcomes: Chiropractic treatment aimed to reduce pain, muscle hypertonicity and restore spinal mobility. Treatment consisted of thermal ultrasound therapy, cervical manipulation with a high-velocity, low-amplitude force, and skin to skin contact manual adjustment. As the result of 12-month treatment, the patient experienced a resolution of neck pain and headache. He reported a reduced headache score from 8 to 0 on a scale of 10. His NDI reduced from 84 % to 8%, and cervical lordosis was restored from 3° to 20° as measured by the Cobb angle between the inferior endplate of C2 to the inferior endplate of C7.
Conclusion: This case report details the long-term recovery of a patient with NF1 from severe headaches and neck pain following chiropractic treatment. It provides evidence and highlights the value of chiropractic intervention in improving neuromuscular functions and resolving cervicogenic headache in a patient with NF1, especially when the problems cannot be effectively solved by pharmacological or other conservative means. Chiropractic manipulative therapy may be a viable option as conservative management of musculoskeletal dysfunction resulting from NF1.
This case highlights the progression of text neck, which was insufficiently treated in a young man. The patient subsequently underwent nine months of chiropractic intervention. He reported resolution of pain and neurological symptoms in the neck and shoulder and regained neck mobility, which were supported by the improvement of radiographic and electromyological findings. Surgery is usually not indicated for mechanical causes of neck pain, unless there are progressive neurologic deficits or intractable pain and disability that is unresponsive to conservative treatments [2]. Avoiding prolonged texting along with maintaining a correct position are keys in preventing or addressing text neck [7].
Case Report
A 24-year-old male YouTuber presented with head and neck pain and paresthesia of the right upper limb for 12 months. He denied any injury event. During the past three years, the patient regularly edited blogging and videos on the YouTube website. He relied heavily, at least 16 hours a day, on a smartphone for both job resources and personal tasks. He would check his screen every 10 minutes. One year prior to this diagnosis, the patient experienced similar symptoms and visited his family physician. Cervical radiographs (Fig. 1) exhibited reduced cervical lordosis, axial rotation of the C5 vertebra, and degenerative proliferation of facets (white arrows) and uncovertebral joints (yellow arrows), suggestive of cervical spondylosis. Previous management included pain medication and muscle relaxants. Interventions included repeated physical therapy, cervical traction, and acupuncture, with some temporary relief. However, 12 months later, the patient repeatedly experienced severe flare-ups of the symptoms. This time, the patient could keep his head up for only a minute and was unable to move his neck without pain. These new difficulties forced him to seek chiropractic attention.
Discussion
Mobile texting and gaming is a growing lifestyle and health concern, with the constant growth in mobile/smartphone usage and adoption. Researches [9,10] revealed that the distinct cervical flexion seen in heavy smartphone users is causing a new overuse condition known as “text neck.” The fulcrum for flexion in the cervical spine in adults is at the C5/C6 level [2]. A neck flexion of 0° to 15° is akin to having the head squarely over the shoulders, wherein the stress on the cervical muscles is acceptably low [9]. A static and flexed neck posture can cause continuous strain of the posterior cervical musculature (the cervical erector spinae and suboccipital muscles, levator scapulae, and semispinalis and trapezius muscles), producing tension headaches, neck and shoulder pain, temporomandibular joint pain, and decreased cervical and upper thoracic ranges of motion [11]. Sustained flexed stress can also slacken posterior ligamentous structures, resulting in instability between vertebral segments, degenerative spondylosis, and vertebral body sliding [2,11]. In the long term, text neck can lead to plastic changes within the nervous system, causing sensorimotor integration deficiencies and further dysfunction [11].
When the neck is in flexion position, the paraspinal muscles act as antagonistic muscles to maintain compliance of the posture, which results in increased myoelectric activity [12]. Surface electromyography (sEMG) is a reliable technique to evaluate muscle activity. Applying two handheld recording electrodes on both sides of the spine 4 cm apart, static sEMG will record and process the level of muscle guarding quantitatively. The signal amplitude of sEMG is positively related to the amount of force produced by the muscles. The levels of muscle tension are displayed with the length and color of the bars in the schematic representation. The sum of all muscle activity readings (in microvolts) for both sides at all levels of the spine is referred to as the electrophysiological (EP) stress score (Fig. 3). In the present study, sEMG was used to assess the myoelectric activity of the paraspinal muscles in the patient with text neck syndrome before and after treatment. It was found that the signal amplitude and EP stress score were significantly different before and after the 9-month chiropractic therapy and were significantly correlated with symptom relief and cervical curvature correction, suggesting that sEMG could be used to objectively assess muscle functional change.
A long-lasting neck flexion due to excessive texting on a smartphone was assumed to be hazardous to cervical structures. Researchers have observed that 10 minutes of static flexion can lead to changes in mechanical and neuromuscular behavior of the cervical spine, potentially leading to decreased strength of cervical spine structures [13]. Surgery is usually not indicated for mechanical causes of neck pain, unless there are progressive neurologic deficits or intractable pain and disability that is unresponsive to conservative treatments [2]. Manual therapy has been shown to have a clinical benefit in correcting reversed cervical curvature [4,6,14]. Treatments for text neck syndrome should target neck problems and be tailored for individual patients based on their treatment responses. Regarding the current case, extension traction therapy is designed to target the anterior longitudinal ligament that attaches to the front of each vertebra. The viscoelastic properties of ligament fibers allow them to accommodate sustained loads. It is presumed that the restoration of natural cervical lordosis following extension traction therapy is mostly due to ligamentous creep (stretching) [15]. Text neck is an altogether preventable overuse degeneration that must be brought into high awareness for smartphone users [11].
Conclusion: In conclusion, the current study reported a progression of text neck, which has been insufficiently treated. Sustained flexion of the neck will cause cervical spine distortion. The improvement of neurologic symptoms has been shown to correlate with radiographic and electromyological alterations responding to the correction of cervical misalignment.
Discussion: Smart clinics employ a new generation of information technologies, such as technological enablement, digitalization, automation, artificial intelligence, telemedicine, virtual reality, and robotic rehabilitation equipment, to completely revolutionize the existing medical system, making it more efficient, easy, and personalized.
Conclusion: This paper reviews the characteristics of smart clinics and evaluate the prospects for smart clinic owners.
血管胸廓出口綜合徵:病例報告
Eric Chu
King Yi Leung
Lucina Lo Wah Ng
Ada Yuk Yin Lam
胸廓出口綜合徵,保守治療
目的:探討一例血管性胸廓出口綜合徵患者的脊醫治療。
臨床特徵: 一名 30 歲男性報告右手突然出現間歇性麻木、緊繃和無力。表現為右上肢皮膚片狀剝落,右肩紫紺;以及冰冷蒼白的右手。運動被確定為激發運動。骨科檢查顯示艾倫測試呈陽性,而 Adson 測試結果有所改變。他的右肘/腕屈肌和伸肌的運動強度為 4/5,右側第 5 掌骨的屈肌和外展肌明顯弱於左側。他之前曾被神經科醫生診斷出患有胸動脈出口綜合徵,並給他開了肌肉鬆弛劑、物理治療運動、按摩治療和針灸治療。
干預和結果:治療方案包括脊柱推拿療法、熱超聲檢查、器械輔助軟組織鬆動和伸展加壓牽引。他的症狀完全消失了,他反復進行的胸廓出口綜合徵和頸椎前凸的骨科檢查都正常。
結論:一名 30 歲男性血管胸廓出口綜合徵通過脊醫治療。
參考
1. Jones MR, Prabhakar A, Viswanath O, et al. Thoracic outlet syndrome: a comprehensive review of pathophysiology, diagnosis, and treatment. Pain Ther 2019;8(1):5-18
2. Sanders RJ, Hammond SL, Rao NM. Diagnosis of thoracic outlet syndrome. J Vascular Surg 2007;46(3):601-604
3. Huang JH, Zager EL. Thoracic outlet syndrome. Neurosurg2004;55(4):897-903
4. Lo CC, Bukry SA, Alsuleman S, Simon JV. Systematic review: The effectiveness of physical treatments on thoracic outlet syndrome in reducing clinical symptoms. Hong Kong Physiother J 2011;29(2):53-63
5. Qaja E, Honari S, Rhee R. Arterial thoracic outlet syndrome secondary to hypertrophy of the anterior scalene muscle. J Surg Case Rep 2017;2017(8)
6. Thompson JF, Jannsen F. Thoracic outlet syndromes. Br J Surg 1996;83(4):435-436
7. Yuschak E, Haq F, Chase S. A case of venous thoracic outlet syndrome: primary care review of physical exam provocative tests and osteopathic manipulative technique considerations. Cureus 2019;11(6)
8. Povlsen S, Povlsen B. Diagnosing thoracic outlet syndrome: current approaches and future directions. Diagnostics 2018;8(1):21
9. Murphy DR, Hurwitz EL, Gregory A, Clary R. A nonsurgical approach to the management of patients with cervical radiculopathy: a prospective observational cohort study. J Manipulative Physiol Ther 2006;29(4):279-287
10. Chu EC, Chan AK, Lin AF. Pitting oedema in a polio survivor with lumbar radiculopathy complicated disc herniation. J Family Med Prim Care.2019;8(5):1765-1768
11. Kim J, Sung DJ, Lee J. Therapeutic effectiveness of instrument-assisted soft tissue mobilization for soft tissue injury: mechanisms and practical application. J Exerc Rehabil 2017;13(1):12-22
12. Chu EC, Lim T, Mak K. Cervical Radiculopathy alleviating by manipulative correction of cervical hypolordosis. J Med Cases 2018;9(5):139-141
13. Berry RH, Oakley P, Harrison DE. Alleviation of radiculopathy by structural rehabilitation of the cervical spine by correcting a lateral head translation posture (-TXH) using Berry translation as a part of CBP Methods. A case report. Chiropr J Australia 2017;45(1):63-72
14. Hooper TL, Denton J, McGalliard MK, Brismée J, Sizer PS Jr. Thoracic outlet syndrome: a controversial clinical condition. Part 1: anatomy, and clinical examination/diagnosis. J Man Manip Ther 2010;18(2):74-83
15. Sanders RJ, Pearce WH. The treatment of thoracic outlet syndrome: A comparison of different operations. J Vasc Surg 1989;1 0(6):626-634
16. Jones MR, Prabhakar A, Viswanath O, et al. Thoracic outlet syndrome: a comprehensive review of pathophysiology, diagnosis, and treatment. Pain Ther 2019;8(1):5-18
Abstract: Objective -To summarize the key findings of the 2021 Survey of the Hong Kong Chiropractic Profession given to Hong Kong chiropractors and compare them to the practice patterns seen in similar local and international studies.
Method: A 52-question survey was conducted online, and access was provided via an email, Facebook, or WhatsApp invitation. The survey was sent to all registered chiropractors in Hong Kong and those on the database at the Chiropractic Doctors Association of Hong Kong, Hong Kong Chiropractic Association, and China Hong Kong Macau Chiropractic Association. The questions were divided into sections into the following areas: information about the typical chiropractic practitioner, chiropractic practice management, chiropractor beliefs, and chiropractor clinical management.
Summary: 80 chiropractors responded to the survey. The results indicate that the typical chiropractor in Hong Kong has a monthly income of $150,000-$300,000 HKD (19,230-38,460USD/month) and is an employee or sole practitioner with a thriving practice. Findings also suggest that the majority of chiropractors in Hong Kong have a vertebral subluxation focus and use a range of techniques in their practice.
Indexing Terms: chiropractic; Hong Kong; survey; practitioner income; practitioner beliefs.
Cite: Leung K, Chu ECP. 2021 Hong Kong Chiropractic Survey: Analysis of Data. Asia-Pac Chiropr J. 2021;2.3. URL apcj.net/papers-issue-2-3/#LeungChuHongKong
Resolution of Gastroesophageal Reflux Disease Following Correction for Upper Cross Syndrome-A Case Study and Brief Review
Upper cross syndrome (UCS) is a condition caused from prolonged poor posture manifesting as thoracic hyperkyphosis with forward head and shoulder postures. It has been associated with several other secondary conditions, causing pain and discomfort to those with the condition. This is a case report of a 35-year-old female presenting to clinic with a sharp pain in the neck, upper back, and sternum area for 4 weeks and gastroesophageal reflux disease (GERD). She had been working at home for several months after the shelter at home order was issued. Following evaluation and corrective treatment with cervical adjustment and soft tissue massage, the patient’s posture improved and reported full pain resolution. Her symptoms of GERD concurrently resolved as well. She continued to receive chiropractic adjustment two times per month for correcting spinal misalignment. Full restoration of posture was attained on the full spine radiographs at 9 months follow-up. The patient remained symptom-free at 12 months follow-up. Manipulative and preventive therapies aimed at treating and preventing UCS should be more widely adopted to prevent secondary conditions.
Keywords: chiropractic manipulation; forward head; forward shoulder posture; gastroesophageal reflux disease; hyperkyphosis; upper cross syndrome.
References
Vakili L., Halabchi F., Mansournia M.A., Khami M.R., Irandoost S., Alizadeh Z. Prevalence of common postural disorders among academic dental staff. Sports Med. 2016;7:e29631. doi: 10.5812/asjsm.29631. – DOI – PMC – PubMed
Han J., Park S., Kim Y., Choi Y., Lyu H. Effects of forward head posture on forced vital capacity and respiratory muscles activity. J. Phys. Ther. Sci. 2016;28:128–131. doi: 10.1589/jpts.28.128. – DOI – PMC – PubMed
Lee S.T., Moon J., Lee S.H., Cho K.H., Im S.H., Kim M., Min K. Changes in activation of serratus anterior, trapezius and latissimus dorsi with slouched posture. Ann. Rehabil. Med. 2016;40:318–325. doi: 10.5535/arm.2016.40.2.318. – DOI – PMC – PubMed
Raine S., Twomey L.T. Head and shoulder posture variations in 160 asymptomatic women and men. Arch. Phys. Med. Rehabil. 1997;78:1215–1223. doi: 10.1016/S0003-9993(97)90335-X. – DOI – PubMed
Raine S., Twomey L.T. Posture of the head, shoulders and thoracic spine in comfortable erect standing. Aust. J. Physiother. 1994;40:25–32. doi: 10.1016/S0004-9514(14)60451-7. – DOI – PubMed
Moore M.K. Upper crossed syndrome and its relationship to cervicogenic headache. J. Manip. Physiol. Ther. 2004;27:414–420. doi: 10.1016/j.jmpt.2004.05.007. – DOI – PubMed
Bayattork M., Seidi F., Minoonejad H., Andersen L.L., Page P. The effectiveness of a comprehensive corrective exercises program and subsequent detraining on alignment, muscle activation, and movement pattern in men with upper crossed syndrome: Protocol for a parallel-group randomized controlled trial. Trials. 2020;21:1–10. doi: 10.1186/s13063-020-4159-9. – DOI – PMC – PubMed
Morris C.E., Bonnefin D., Darville C. The Torsional Upper Crossed Syndrome: A multi-planar update to Janda’s model, with a case series introduction of the mid-pectoral fascial lesion as an associated etiological factor. J. Bodyw. Mov. Ther. 2015;19:681–689. doi: 10.1016/j.jbmt.2015.08.008. – DOI – PubMed
Kim E.K., Kim J.S. Correlation between rounded shoulder posture, neck disability indices, and degree of forward head posture. J. Phys. Ther. Sci. 2016;28:2929–2932. doi: 10.1589/jpts.28.2929. – DOI – PMC – PubMed
Isabel de-la-Llave-Rincón A., Puentedura E.J., Fernández-de-Las-Peñas C. Clinical presentation and manual therapy for upper quadrant musculoskeletal conditions. J. Man. Manip. Ther. 2011;19:201–211. doi: 10.1179/106698111X13129729551985. – DOI – PMC – PubMed
Bae W.S., Lee H.O., Shin J.W., Lee K.C. The effect of middle and lower trapezius strength exercises and levator scapulae and upper trapezius stretching exercises in upper crossed syndrome. J. Phys. Ther. Sci. 2016;28:1636–1639. doi: 10.1589/jpts.28.1636. – DOI – PMC – PubMed
Hidalgo B., Hall T., Bossert J., Dugeny A., Cagnie B., Pitance L. The efficacy of manual therapy and exercise for treating non-specific neck pain: A systematic review. J. Back Musculoskelet Rehabil. 2017;30:1149–1169. doi: 10.3233/BMR-169615. – DOI – PMC – PubMed
Seidi F., Bayattork M., Minoonejad H., Andersen L.L., Page P. Comprehensive corrective exercise program improves alignment, muscle activation and movement pattern of men with upper crossed syndrome: Randomized controlled trial. Sci. Rep. 2020;10:20688. doi: 10.1038/s41598-020-77571-4. – DOI – PMC – PubMed
Ruivo R.M., Pezarat-Correia P., Carita A.I. Effects of a Resistance and Stretching Training Program on Forward Head and Protracted Shoulder Posture in Adolescents. J. Manip. Physiol. Ther. 2017;40:1–10. doi: 10.1016/j.jmpt.2016.10.005. – DOI – PubMed
Fathollahnejad K., Letafatkar A., Hadadnezhad M. The effect of manual therapy and stabilizing exercises on forward head and rounded shoulder postures: A six-week intervention with a one-month follow-up study. BMC Musculoskelet Disord. 2019;20:86. doi: 10.1186/s12891-019-2438-y. – DOI – PMC – PubMed
Ghanbari A., Ghaffarinejad F., Mohammadi F., Khorrami M., Sobhani S. Effect of forward shoulder posture on pulmonary capacities of women. Sports Med. 2008;42:622–623. doi: 10.1136/bjsm.2007.040915. – DOI – PubMed
Watson D.H., Trott P.H. Cervical headache: An investigation of natural head posture and upper cervical flexor muscle performance. Cephalalgia. 1993;13:272–284. doi: 10.1046/j.1468-2982.1993.1304272.x. – DOI – PubMed
Huang M.H., Barrett-Connor E., Greendale G.A., Kado D.M. Hyperkyphotic posture and risk of future osteoporotic fractures: The Rancho Bernardo study. J. Bone Miner. Res. 2006;21:419–423. doi: 10.1359/JBMR.051201. – DOI – PMC – PubMed
Singla D., Veqar Z. Association between forward head, rounded shoulders, and increased thoracic kyphosis: A review of the literature. J. Chiropr. Med. 2017;16:220–229. doi: 10.1016/j.jcm.2017.03.004. – DOI – PMC – PubMed
Chronic orchialgia can be the result of pathological processes of the scrotal contents or stem from non-intrascrotal structures. Successful pain management depends on identifying the source of localized or referred pain. This is a case report of a 39-year-old male sports coach who presented with low back pain, right orchialgia, and sciatica refractory to conservative management. Magnetic resonance (MR) imaging revealed disc protrusion at L3/L4 and L4/L5 levels. Positive outcomes in relieving back and testicular pain were obtained after a total of 30 chiropractic sessions over a 9-week period. The evidence of the subjective improvement was corroborated by regression of the herniated discs documented on the repeat MR imaging. While chronic orchialgia is not an uncommon problem for men of all ages, it has seldom been described in association with lumbar discogenic disease. The current study provided preliminary support for a link between orchialgia and lumbar disc herniation. Chiropractic manipulation had provided a mechanistic alleviation of noxious lumbar stimuli, leading to symptomatic and functional improvements.
Keywords: chiropractic; discogenic disease; lumbar disc herniation; orchialgia; testicle.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
REFERENCES
1. Von Gontard A, Cardozo L, Rantell A, Djurhuus JC. Adolescents with nocturnal enuresis and daytime urinary incontinence— How can pediatric and adult care be improved—ICI-RS 2015. Neurourol Urodynam 2017;36:843–849.
2. Adam A, Claassen F, Coovadia A, et al. The South African guidelines on enuresis2017. Afr J Urol 2018;24(1):1-13.
3. Selvaraj PR, Thirumalai R. Late adolescent primary nocturnal enuresis: a case report. Int J Res Med Sci 2017;5(11):5075-5078.
4. Brauge D, Madkouri R, Clement R, et al. What are the possibilities of spontaneous resorption of a thoracic disc herniation occupying more than 20% ofthe spinal canal in the asymptomatic subject? Comparative study. J Clin Neurosci 2017; 44:269-273.
5. Shah A, Botchu R, Grainger MF, et al. Acute symptomatic calcific discitis in adults: a case report and review of literature. Skeletal Radiol 2015;44(12):1819– 1824.
6. Inoue T. Pure conus medullaris syndrome without lower extremity involvement caused by intradural disc herniation at L1/2: a case report. Spine Surg Relat Res 2019;3:392–395.
7. Nene Y, Jilani TN. Neuroanatomy, conus medullaris. In: StatPearls, Internet. Treasure Island, FL: StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545227/.
8. Brouwers E, van de Meent H, Curt A, et al. Definitions of traumatic conus medullaris and cauda equina syndrome: a systematic literature review. Spinal Cord 2017;55:886–890.
9. Rider IS, Marra EM. Cauda equina and conus medullaris syndromes. In: StatPearls, Internet. Treasure Island, FL: StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537200/.
10. Yeung CK, Sit FK, To LK, et al. Reduction in nocturnal functional bladder capacity is a common factor in the pathogenesis of refractory nocturnal enuresis. BJU Int 2002;90(3):302–307.
11. Siracusa G, Sparacino A, Lentini VL. Neurogenic bladder and disc disease: a brief review. Curr Med Res Opin 2013;29(8):1025–1031.
12. Reed WR, Beavers S, Reddy SK, Kern G. Chiropractic management of primary nocturnal enuresis. J Manipulative Physiol Ther 1994;17:596–600.
13. van Poecke AJ, Cunliffe C. Chiropractic treatment for primary nocturnal enuresis: a case series 33 consecutive patients. J Manipulative Physiol Ther 2009; 32:675– 81.
14. Instebø E, Lystad RP. Chiropractic care of an 8-year-old girl with nonorganic, primary nocturnal enuresis: a case report. J Chiropr Med 2016;15:47–52.
15. Chu ECP, Chakkaravarthy DM, Lo FS, Bhaumik A. Regression of lumbar disc herniation following nonsurgical treatment. Eur J Mol Clin Med 2020;7(1): 27– 29.
Rheumatoid arthritis (RA) is an autoimmune disease that affects the synovial tissue which lines joints and tendons. The craniocervical junction is made up exclusively of synovial joints and ligaments and especially vulnerable to the inflammatory process of RA. The chronic inflammation of RA leads to loss of ligamentous restriction and erosion of the bony structures and results in craniocervical instability (CCI). This is a case report of an 80-year-old woman who had been diagnosed with seropositive RA two decades ago presented with head dropping and losing balance while walking for several months. Radiographic images of the cervical spine showed RA-related features of instability in the form of atlantoaxial instability, cranial settling and subaxial subluxation. Since physical therapy and acupuncture previously failed to provide a substantial, long-lasting outcome, the patient sought chiropractic care for her condition. The chiropractic regimen consisted of upper thoracic spine mobilization/adjustment, electrical muscle stimulation of the cervical extensors, home exercises and neck bracing. She regained substantial neck muscle strength, gaze angle and walking balance following a 4-month chiropractic treatment, although cervical kyphosis persisted. The current study aims to provide basic knowledge of CCI associated with RA and ability to modify a treatment program to accommodate the needs of patients with coexisting red flags.
Keywords: Cervical spine; chiropractic; craniocervical instability (CCI); head dropping; rheumatoid arthritis (RA).
2021 AME Case Reports. All rights reserved.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/acr-20-131). The authors have no conflicts of interest to declare.


Degenerative disease of the lumbar spine is often ignored as a potential cause of testicular pain because the exact link between the two remains uncertain. This article reports the case of a 60-year-old man with a 3-year history of low back pain and unexplained right testicular pain for 2 years. Painful symptoms were negatively affecting his social, physical, and sexual functions. After failure to achieve pain relief through multiple types of therapy, the patient sought chiropractic treatment for his condition. Lumbar spine magnetic resonance imaging (MRI) revealed disc protrusion at the L1/L2, L3/L4, and L4/L5 segments causing thecal sac indentations. Due to the absence of direct testicular causes, the medical impression was chronic testicular pain (CTP) complicating lumbar disc disease. The patient experienced regular improvement in his low back and testicular pain with complete resolution of both after 8 weeks of chiropractic treatment. This article describes an overlook of the etiology of this patient’s testicular pain and a successful option in treating the patient. CTP has multifactorial etiology. An excellent treatment outcome depends heavily on recognizing the origin of the pain.
Regression of Lumbar Disc Herniation Following Non-surgical Treatment
Eric Chun-Pu Chu, Divya Midhun Chakkaravarthy, Fa-Sain Lo, Amiya Bhaumik.
Abstract Key words: Chiropractic, herniated disc regression, lumbar disc herniation, non-surgical treatment
| |||
</div

First Published July 1, 2020 Case Report
| Article information |
Open Access
Atlantoaxial rotatory subluxation (AARS) is the loss of normal alignment and stability of the first (atlas) and second (axis) cervical vertebrae with respect to each other. We describe the clinical challenges of managing a 10-year-old boy who presented with repetitive episodes of torticollis. Open-mouth odontoid radiograph and computed tomographic (CT) scan gave a diagnosis in ARRS, based on its characteristic imaging findings. The child was admitted multiple times for continuous halter traction in the first 6 months after symptom onset. He also experienced a temporary complication from an overcorrection with correcting neck bracing. Seven months after symptom onset, this case was discussed by a multidisciplinary spine team and referred to chiropractic clinic. Despite persistent radiographic evidence of atlantoaxial instability, after 5 months of chiropractic treatment, the child was asymptomatic with nearly full range of neck movement. He also weaned off acetaminophen he had been taking over the past year. Incidentally, bilateral gynecomastia was discovered at the surveillance after treatment. The incidental finding of innocent gynecomastia, even if common in preteen boys, brings up the topic of acetaminophen’s effects on the regulation of sex hormones that was previously overlooked.

Chiropractic Telemedince Guideline
To: 食物及衞生局局長
香港添馬添美道2號政府總部東翼18樓
CC: 香港灣仔皇后大道東182號
香港脊醫管理局及委員會辦公室
陳肇始教授:
Chiropractic Telemedince Guideline
新病毒擴大,遠程醫療將會變成未來趨勢。患者如果可以通過電話或視像會議與脊醫聯繫,進行各種遠端看診,以避免民眾到診所引發的人際傳染風險,也大幅提高對患者的醫療服務。
香港醫務委員會在二零一九年十二月已公布了遠程醫療指引, 本會現就建議香港脊醫管理局可立即設立制度和相關指引, 積極引進及推動遠程醫學,以加強脊醫學教育、診斷及治療工作的效率。
遠程醫療應用範圍廣泛,可透過資訊科技分析病歷、視像診症、診症分流,甚至遠距離護理、遙距教育等,病人足不出戶,便可接受脊醫評估,減省輪候時間,亦能妤緩醫療人手及服務不足以應付需求的壓力。
香港脊醫遠程醫療指引也可以做到以下的功能:
(一) 脊醫可以使用遠程醫學設備,討論及會診,節省卻轉運病人的時間,減少交叉感染,令病人和家人得到及時的治療和關懷。
(二)脊醫可和醫院系統接軌,在不同的地點會診門診的病人。
(三)脊醫科生可以在教學上觀察病人,學習臨床醫學。
(四)可加入國際專家會診。
本會促請閣下積極設立及推動遠程醫學,讓更多註冊脊醫履行醫務責任。
專此奉達,敬候赐覆。
朱君璞脊醫 (香港執業脊醫協會主席)
二零二零年三月二十六日
 Chiropractic Telemedince Guideline
Chiropractic Telemedince Guideline
CDAHK Record on Continuing Professional Development (CPD) Activities
(for the period from 1-1-2019 to 31-12-2019 )


A variety of age-related problems, including salivary secretory disorders, poor oral motor coordination, neuromuscular weakness, neurodegenerative diseases, stroke, and structural changes, can result in swallowing disorders. Given that causes of dysphagia differ from patient to patient, individualized treatment plans tailored toward patients’ specific conditions are needed. Here we present a case of an elderly woman with upper neck stiffness and dysphagia sought chiropractic treatment. Radiographic findings suggested cervical spondylosis with a vertical atlantoaxial subluxation. Following 20 sessions of chiropractic treatment, the patient experienced complete relief from neck problems and difficulty in swallowing. Rhythmic swallowing movements are controlled by a central pattern-generating circuit of the brain stem. In this case, the brain stem could have been compressed by the odontoid process of the axis due to C1/2 instability. Cervicogenic dysphagia is a cervical cause of difficulty...






We report a 58-year-old male with sequelae of polio who presented with low back and left buttock pain, and pitting oedema of both legs for four months. The patient had a history of poliomyelitis at the age of 1 year which resulted in bilateral lower leg weakness, particularly on the left side. Magnetic resonance imaging showed cervical spinal stenosis secondary to posterior osteophyte formation, left paracentral disc extrusion at L2/L3 and L3/L4 levels with compression of the traversing L4 nerve root. The findings confirmed a diagnosis of lumbar radiculopathy caused by a herniated disc. The patient subsequently underwent a chiropractic treatment. The painful symptoms and pitting oedema in this case resolved with spinal adjustment in addition to scraping therapy to strengthen bilateral low back and the gluteal muscles. This case provides circumstantial evidence of a scarcely mentioned association between pitting oedema and lumbar radiculopathy caused by disc herniation. The pathophysiological mechanism is elusive, but might involve a complexity of cytokine-mediated inflammation and interconnection between somatic and autonomic nervous systems.



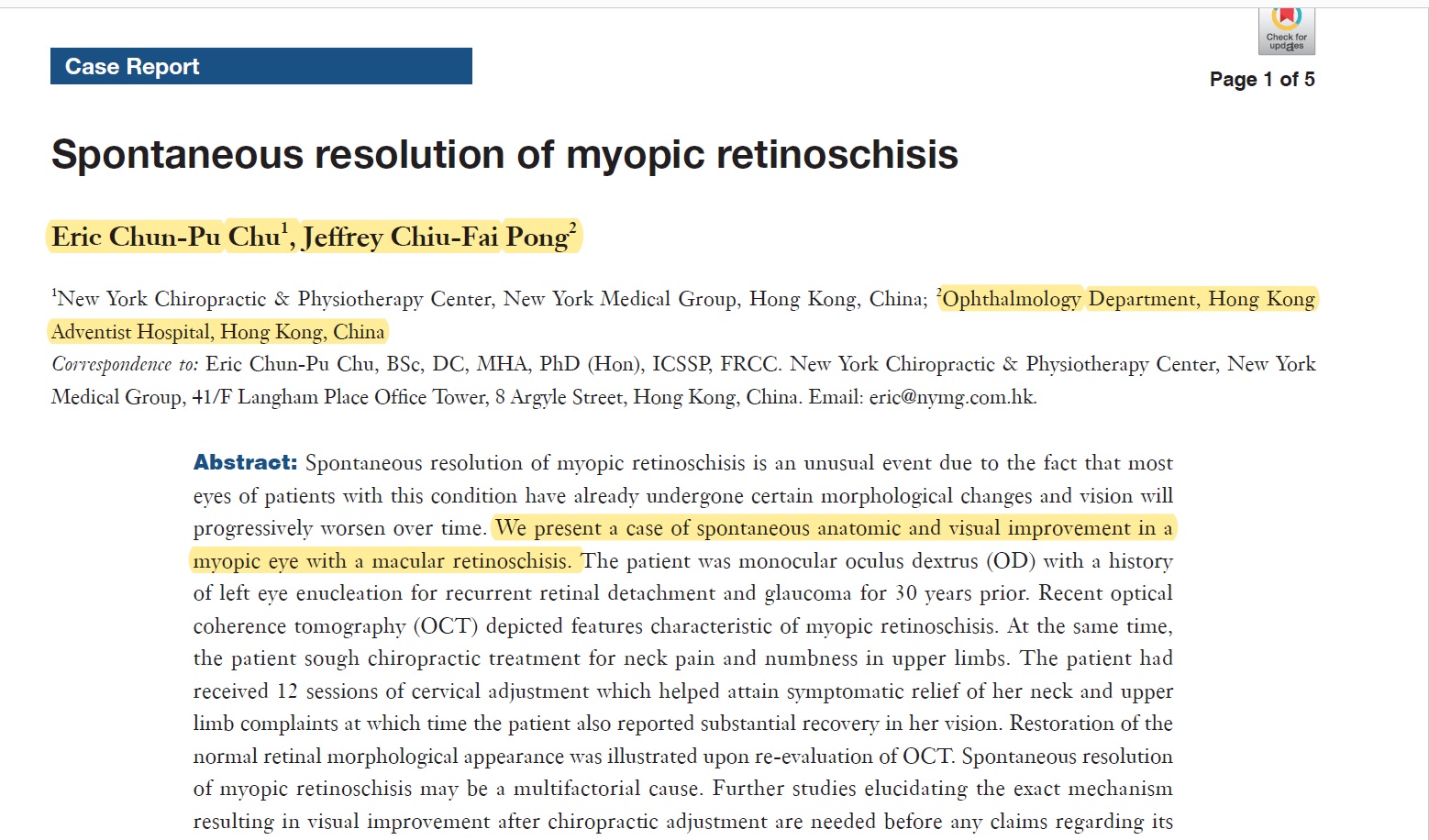
Dr. Eric Chun Pu CHU had published a case on Spontaneous resolution of myopic retinoschisis after Chiropractic Care












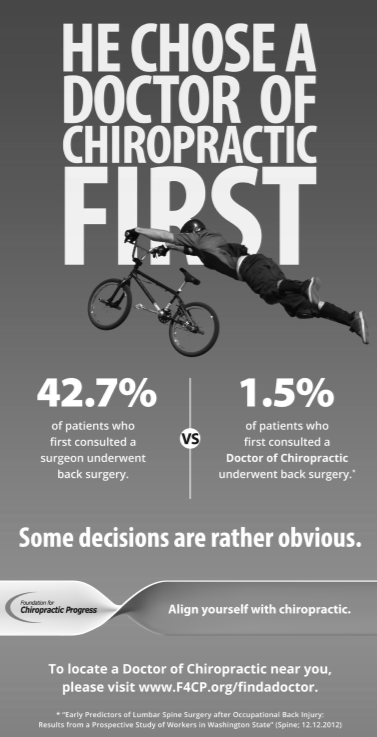
Great News! The F4CP’s ad appears today on page D3 of the Wall Street Journal. Be sure to pick up a copy and share this news with your peers!